Poslink Issue 90, Autumn 2020
HIV criminalisation increases stigma and inhibits testing, treatment care and support.
After years of progress there are still many areas of criminal and public health law that impact people living with HIV in Australia.
In this edition, we have asked Vixen Collective to revisit laws that continue to criminalise sex workers based on HIV status. Our contributors also tackle the troubling spread of ‘spit-and-test’ laws and how people living with HIV negotiate disclosure, sex and ‘reasonable precautions’ for prevention.
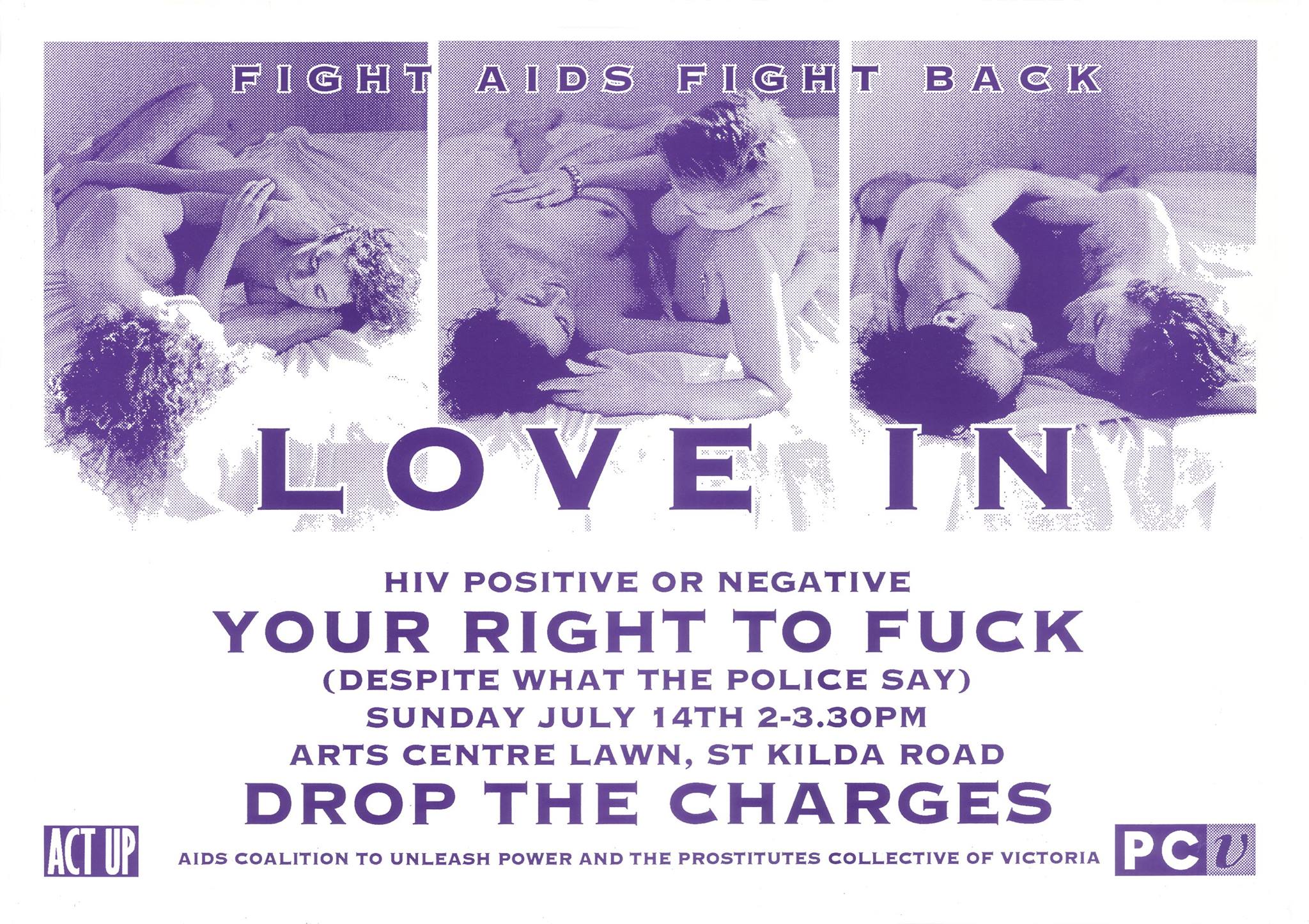
Feature image: Sex workers and sex workers’ representative organisations have a long history of calling for equal protection before the law, including the removal of HIV criminalisation. Pictured: poster for a ‘Love In to Drop the Charges’ organised by the Prostitutes Collective of Victoria and ACT-UP on July 14, 1992 in Melbourne. Courtesy of the Australian Lesbian and Gay Archives poster collection.